What Is Heart Failure
Heart failure, also known as congestive heart failure, is a State in which your heart’s muscle doesn’t pump blood well enough. Some conditions, such as heart narrowed arteries (coronary artery disease) or, gradually makes your heart too weak or stiff to fill and pump efficiently.
If you have heart failure, you’re not alone. About 5.7 million Americans are living with it today. In fact, it’s one of the most common reasons people age 65 and older go into the hospital. It can take years for heart failure to develop. About 91% of CHF sufferers have a medical history involving hypertension. I know this can be a difficult topic for people to read about, but please read all the way to the end because there is hope.
So if you don’t yet have heart failure but are at risk of it, you should make lifestyle changes now to prevent it! Heart failure symptoms usually develop over time as your heart becomes weaker and less able to pump the blood that your body needs. Heart failure usually results in an enlarged heart (left ventricle).
Anatomy of Your Heart and Circulatory System
The right side of the heart pumps blood to the lungs while the left side pumps blood to the rest of the body. Blood from the body enters the right atrium through the vena cava. It then flows into the right ventricle where it is pumped to the lungs through the pulmonary artery, which carries deoxygenated blood to the lungs.
In the lungs, oxygen is loaded onto red blood cells and returns to the left atrium of the heart via the pulmonary veins. Blood then flows into the left ventricle where it is pumped to the organs and tissues of the body. Oxygen is downloaded from red blood cells into the various organs while carbon dioxide, a waste product of metabolism, is added to be removed from the lungs.
Blood then returns to the right atrium to start the cycle again. The pulmonary veins are unusual in that they carry oxygenated blood, while the pulmonary artery carries deoxygenated blood. This is a reversal of duties versus the roles of veins and arteries in the rest of the body.
Heart Failure develops when your ventricles can’t pump blood in sufficient volume to the body. Eventually, blood and other fluids can back up inside your:
- Lungs
- Abdomen
- Liver
- Lower Extremities
If you would like to get a quick introduction, instead of reading on, we have found a great video for you to watch:
Causes of Congestive Heart Failure
Heart failure often develops after other conditions have damaged or weakened your heart. However, the heart doesn’t need to be weakened to cause heart failure. It can also occur if the heart becomes too stiff.
In heart failure, the main pumping chambers of your heart (the ventricles) may become stiff and not fill properly between beats. In some cases of heart failure, your heart muscle may become damaged and weakened, and the ventricles stretch (dilate) to the point that the heart can’t pump blood efficiently throughout your body.
Over time, the heart can no longer keep up with the normal demands placed on it to pump blood to the rest of your body.
An ejection fraction is an important measurement of how well your heart is pumping and is used to help classify heart failure and guide treatment. In a healthy heart, the ejection fraction is 50 percent or higher — meaning that more than half of the blood that fills the ventricle is pumped out with each beat.
But heart failure can occur even with a normal ejection fraction. This happens if the heart muscle becomes stiff from conditions such as high blood pressure.
Heart failure can involve the left side (left ventricle), right side (right ventricle) or both sides of your heart. Generally, heart failure begins with the left side, specifically the left ventricle — your heart’s main pumping chamber.
What are the Most Common Types of Heart Failure
Left-sided CHF is the most common type of CHF. It occurs when your left ventricle doesn’t properly pump blood out to your body. As the condition progresses, fluid can build up in the lungs, which makes breathing difficult.
There are two kinds of left-sided heart failure:
- Systolic heart failure occurs when the left ventricle fails to contract normally. This reduces the level of force available to push blood into circulation. Without this force, the heart can’t pump properly.
- Diastolic failure, or diastolic dysfunction, happens when the muscle in the left ventricle becomes stiff. Because it can no longer relax, the heart can’t quite fill with blood between beats.
Right-sided CHF occurs when the right ventricle has difficulty pumping blood to your lungs. Blood backs up in your blood vessels, which causes fluid retention in your lower extremities, abdomen, and other vital organs.
The Stages of Congestive Heart Failure
Congestive Heart Failure doesn’t happen in a day; it usually takes years to develop. To help stage patients and their treatments correctly, doctors use a four-stage classification of Congestive Heart Failure. Certain mechanisms happening inside the body accompanies each stage, but what matters to us is what we can see outside, as symptoms and therefore, how seriously we need to take them.
The stages of Congestive Heart Failure based on this approach are:
- Stage A: Risk factors for the decrease in ejection fraction (e.g. hypertension)
- Stage B: Reduced ejection fraction but NO symptoms
- Stage C: Reduced ejection fraction plus symptoms
- Stage D:Symptoms with ANY activity or even at rest, ie “end-stage heart failure.”
What are the Symptoms of Congestive Heart Failure?
People with a history of cardiovascular health issues or several risk factors for CHF should seek immediate care if they experience symptoms of CHF. Similarly, if symptoms do not improve after a few days, a person should see a doctor.
The Most Common Symptoms of CHF are:
- Shortness of breath or difficulty breathing: People with CHF may also struggle to breathe when lying down due to fluid accumulation in the lungs.
- A persistent, unexplained cough: Some people experience wheezing and pink or blood-stained mucus.
- Swelling in the legs, ankles, abdomen, or hands: The swelling may get worse as the day goes on or after exercise.
- Feeling tired: This can happen even when someone is well-rested.
- Changes in thinking and memory: Electrolyte imbalances due to CHF can impair the ability to think clearly.
- Nausea: This can be accompanied by a drop in appetite.
- A rapid heart rate: This occurs because the heart is unable to pump blood with a regular rhythm.
- Feeling light-headed or dizzy: This might also include tingling or numbness in the extremities due to an inadequate blood supply.
- As fluid builds up, people with CHF may develop painful swelling. This is called edema and was once referred to as dropsy.
- Swelling caused by CHF can undermine movement, and may even cause dangerous blood clots in the legs. Also, organs affected by fluid retention may not work properly, making it harder to breathe or exercise.
- Children with CHF may experience delays in physical development, while babies with the condition may struggle to gain weight.
What are the Risk Factors for Congestive Heart Failure
Common risk factors for developing congestive heart failure include:
- Coronary artery disease
- Heart attack
- High blood pressure
- A history of significant heart valve disease
- An enlarged heart
- Obesity
- Diabetes
Things, like excessive alcohol intake, and using illegal drugs, are all known to damage your heart.
Some things that raise your chances of heart failure are out of your control, including:
- Race (African-Americans are more likely to have heart failure)
- Heart defects you’re born with
- Age (your odds go up if you’re 65 or older)
What are the Treatment Options for CHF?
There are more treatment options available for heart failure than ever before. Tight control over your medications and lifestyle, coupled with careful monitoring, are the first steps. As the condition progresses, doctors specializing in the treatment of heart failure can offer more advanced treatment options.
The goals of treating heart failure are primarily to decrease the likelihood of disease progression (thereby decreasing the risk of death and the need for hospitalization), to lessen symptoms, and to improve quality of life.
Together, you and your doctor can determine the best course of treatment for you.
Doctors usually treat heart failure with a combination of medications. Depending on your symptoms, you might take one or more medications, including:
Medications Used for Treating CHF
Angiotensin-converting enzyme (ACE) inhibitors. These drugs help people with systolic heart failure live longer and feel better. ACE inhibitors are a type of vasodilator, a drug that widens blood vessels to lower blood pressure, improve blood flow and decrease the workload on the heart. Examples include enalapril (Vasotec), lisinopril (Zestril) and captopril (Capoten).
Angiotensin II receptor blockers. These drugs, which include losartan (Cozaar) and valsartan (Diovan), have many of the same benefits as ACE inhibitors. They may be an alternative for people who can’t tolerate ACE inhibitors.
Beta blockers. This class of drugs not only slows your heart rate and reduces blood pressure but also limits or reverses some of the damage to your heart if you have systolic heart failure. Examples include carvedilol (Coreg), metoprolol (Lopressor) and bisoprolol (Zebeta).
Angiotensin Receptor-Neprilysin Inhibitor combination. Enestro is a combination product that contains two medications: sacubitril and valsartan. This combination medication is used with other medicines to treat heart failure when the heart is unable to pump effectively.
These medicines reduce the risk of some abnormal heart rhythms and lessen your chance of dying unexpectedly. Beta-blockers may reduce signs and symptoms of heart failure, improve heart function, and help you live longer.
Other Medications That Help CHF
Diuretics. Often called water pills, diuretics make you urinate more frequently and keep fluid from collecting in your body. Diuretics, such as furosemide (Lasix), also decrease fluid in your lungs so you can breathe more easily.
Because diuretics make your body lose potassium and magnesium, your doctor may also prescribe supplements of these minerals. If you’re taking a diuretic, your doctor will likely monitor levels of potassium and magnesium in your blood through regular blood tests.
Aldosterone antagonists. These drugs include spironolactone (Aldactone) and eplerenone (Inspra). These are potassium-sparing diuretics, which also have additional properties that may help people with severe systolic heart failure live longer.
Unlike some other diuretics, spironolactone and eplerenone can raise the level of potassium in your blood to dangerous levels, so talk to your doctor if increased potassium is a concern, and learn if you need to modify your intake of food that’s high in potassium.
Inotropes. These are intravenous medications used in people with severe heart failure in the hospital to improve heart pumping function and maintain blood pressure.
Digoxin (Lanoxin). This drug also referred to as digitalis, increases the strength of your heart muscle contractions. It also tends to slow the heartbeat. Digoxin reduces heart failure symptoms in systolic heart failure. It may be more likely to be given to someone with a heart rhythm problem, such as atrial fibrillation.
You may need to take two or more medications to treat heart failure. Your doctor may prescribe other heart medications as well — such as nitrates for chest pain, a statin to lower cholesterol or blood-thinning medications to help prevent blood clots — along with heart failure medications. Your doctor may need to adjust your doses frequently, especially when you’ve just started a new medication or when your condition is worsening.
Surgery and Other Procedures to Stabilize CHF
In some cases, doctors recommend surgery to treat the underlying problem that led to heart failure. Some treatments being studied and used in certain people include:
Coronary bypass surgery. If severely blocked arteries are contributing to your heart failure, your doctor may recommend coronary artery bypass surgery. In this procedure, blood vessels from your leg, arm or chest bypass a blocked artery in your heart to allow blood to flow through your heart more freely.
Heart valve repair or replacement. If a faulty heart valve causes your heart failure, your doctor may recommend repairing or replacing the valve. The surgeon can modify the original valve to eliminate backward blood flow. Surgeons can also repair the valve by reconnecting valve leaflets or by removing excess valve tissue so that the leaflets can close tightly. Sometimes repairing the valve includes tightening or replacing the ring around the valve (annuloplasty).
Valve replacement is done when valve repair isn’t possible. In valve replacement surgery, the damaged valve is replaced by an artificial (prosthetic) valve.
Certain types of heart valve repair or replacement can now be done without open heart surgery, using either minimally invasive surgery or cardiac catheterization techniques.
Implantable cardioverter-defibrillators (ICDs). An ICD is a device similar to a pacemaker. It’s implanted under the skin in your chest with wires leading through your veins and into your heart.
The ICD monitors the heart rhythm. If the heart starts beating at a dangerous rhythm, or if your heart stops, the ICD tries to pace your heart or shock it back into normal rhythm. An ICD can also function as a pacemaker and speed your heart up if it is going too slow.
Does The DASH Diet Benefit Individuals With CHF?
Eating a low-sodium diet could produce blood pressure benefits similar to taking anti-hypertension medicine for people with a common kind of heart failure, a small new study suggests.
The research, presented at a meeting of the Heart Failure Society of America and published in the journal Circulation: Heart Failure, showed that three weeks of eating according to the Dietary Approaches to Stop Hypertension — also known as the DASH diet — improved arterial function in elderly people with “diastolic” heart failure.
“Diastolic” heart failure, or heart failure with preserved ejection fraction, occurs when adequate blood is not able to be pumped out of the heart because of heart stiffness. Researchers noted that more than half of older adults with heart failure have this heart-stiffening condition.
“Our work suggests diet could play an important role in the progression of heart failure, although patients should always talk to their doctor before making major dietary changes,” study researcher Dr. Scott Hummel, M.D., a cardiologist at the University of Michigan Frankel Cardiovascular Center, said in a statement.
What Is The Overall Prognosis With CHF Patients?
Heart failure is a chronic, progressive condition, which means it gets worse with time and you cannot move back to a less advanced stage. But even though the condition doesn’t necessarily get better, managing heart failure the right way can help reduce symptoms and slow down the condition.
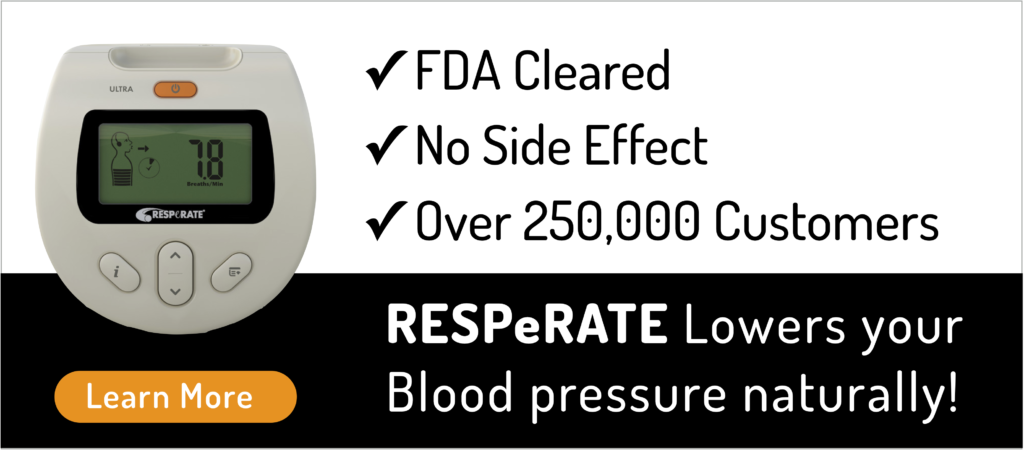
Part of managing heart failure is to ensure you keep your blood pressure in check. Keeping your blood pressure down will decrease the workload that your heart will have to do.
Statistics can be deceiving when you try to apply them to an individual, but congestive heart failure is taken seriously in all of its stages. Prognosis varies greatly, but according to the Cleveland Clinic, the annual mortality rate for people with congestive heart failure is between 5 and 20 percent.
“Patients should understand, the course of their disease has many variables. There are general statistics, but so many factors determine a patient’s life expectancy, and it is difficult to determine a definitive prognosis,” says Aggarwal.
People with congestive heart failure also need to remember statistics don’t necessarily determine your prognosis. “Many patients live long and productive lives with controlled and stable congestive heart failure,” says Marc Leavey, an internist who has treated many patients with congestive heart failure. “Those in the lower stages of failure, if properly managed, can hope to have a near-normal life expectancy.”
Click here for more information about CHF

Reviewed by Alon Gitig, M.D., F.A.C.C.
Dr. Alon Gitig is a senior cardiologist in Mount Sinai Doctors Westchester and an assistant professor of medicine at the Mount Sinai Medical Center.
 Eli Ben-Yehuda
Eli Ben-Yehuda 















 Download Brochure
Download Brochure
Comments
8 Replies to “The Dangerous Link Between Hypertension and Heart Failure”
Thank you for this informative article. I believe one thing not mentioned often enough to assist the heart is proper hydration. A hydrated body helps the heart muscle pump blood through the body more efficiently. The DASH diet helps in this area, since fruits and veggies have a high water density. In addition to DASH and a product like Resperate, additional hydration could be of benefit.
As a regular reader, I appreciate your newsletter, as it helps us all to embark on a more healthy existence. 🙂
Hi Tina, Thank you for that healthy reminder. Kindest Regards, Eli, Content Manager, RESPeRATE.
Okay,overweight,lifestyle,etc are all understandable. Lets go up my road. Ive been fighting blood pressure problems for years.Im on and been on what has turned out to be dangerous bp meds. My problem is anxiety. I can top the levels of high blood pressure. No meditation all do not work. so with keeping in mind.Ive been on valium and some others.Once anxiety and worrying hit. My bp skyrockets. Right now i cant pass a physical for work after a operation that didnt work.My reason is bp.Because im losing everything.Any suggestions.
Hi Dave, Have you considered trying RESPeRATE? It does work and it has a 60-day money back guarantee that if your
not happy with the results you can return for a full refund. Kindest Regards, Eli.
My Resperate device came in the mail today but I am afraid to let my husband use it because he was diagnosed with congestive heart failure three months ago. He had an echocardiogram last week which showed improved heart function. His ejection fraction went up from 30% to 40-45%. He currently has no symptoms and feels good since starting on blood pressure medication three months ago. I didn’t know that this device was not recommended for people with chf when I bought it. I just wish I knew whether or not it would be safe to start using the device.
Hi Emma,Thank you for your question. I have included links to studies done on people with CHF. They discuss how guided breathing helps increase overall cardiac function. Of course you can also discuss this with your cardiologist if you have further concerns, Kindest Regards, Eli, Content Manager, RESPeRATE.
https://www.ahajournals.org/doi/full/10.1161/circheartfailure.108.772640
https://onlinelibrary.wiley.com/doi/epdf/10.1093/eurjhf/hfr090
https://journals.lww.com/jhypertension/Abstract/2015/06001/_PP_36_04____USEFULNESS_OF_SLOW_BREATHING_TRAINING.1487.aspx
I use a resmed machine overnight for sleep apnea. When would I use a Resperate device ? How do they differ?
Does it make sense to use both? My B/P has been hovering in the 180’s over the 90’s. This morning it went higher than the medical office machine could register. They will probably just increase my meds. Again! Any suggestions?
Mary
Hi Mary, You would use RESPeRATE any time during the day before you go to bed. RESPeRATE is for lowering blood pressure
while you CPAP machine is used to help with sleep apnea. So the devices work on separate systems. Kindest Regards Eli,
Content Manager RESPeRATE.